What is breast reduction surgery?
Women who have large breasts may experience a variety of problems from the weight and size of their breasts such as back, neck, shoulder pain, and skin irritation within the breast fold.
The aim of the surgery is often to improve such symptoms. However, improvement of such symptoms is not guaranteed as you may also have additional mechanical reasons for pain in these areas (such as wear and tear on the joints) or a chronic fungal infection of the skin. Some patients seek breast reduction surgery to achieve a greater degree of proportion to their shape, to reduce levels of self-consciousness, or to feel more comfortable wearing certain types of clothes. For others the goal of surgery is to be able to undertake certain activities (such as exercise) more easily.
Breast reduction is therefore primarily a functional procedure aimed at improving the problems detailed above rather than to enhance the appearance of the breasts. As with any cosmetic procedure it is important to have realistic expectations about the results.
HOW IS BREAST REDUCTION SURGERY PERFORMED?
Breast reduction surgery can be performed in a variety of ways but usually involves 2 key elements:
• removal of breast tissue to reduce the overall volume of the breast
• repositioning of the nipple (if it has descended, which is normally the case)
There are a variety of different surgical techniques used to reduce and reshape the female breast. Most techniques rely on excision of skin and breast tissue to reduce breast volume. The nipple is moved to its new location using some of the breast tissue to give it a blood supply to keep it alive (known as a pedicle).
There are multiple different pedicle patterns but the most commonly used are:
• superomedial (below left)
• inferior (below centre)
• superior (below right)
Each pedicle type has a different shape and relies on a different blood supply to keep the nipple alive. Decisions on which pedicle type is used during the procedure relate to the distance the nipple needs to be moved (vertically from its current position to the planned new position), any specific anatomic considerations that need to be accounted for in your particular case and your surgeon’s preference for a particular technique.
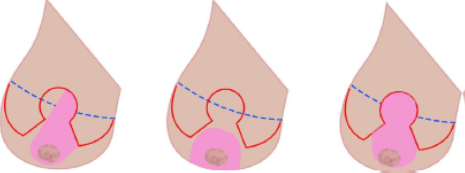
The dashed blue line in the diagram above represents the breast crease (known as the infra mammary fold) and the red lines represent the skin incision lines. The pedicle is shaded pink.
Inverted T or anchor pattern breast reduction with superomedial pedicle:

Top left: This patient presented requesting a breast reduction. She had 34 H cup breasts with the nipple sitting almost at the lowest point of the breast (known as nipple ptosis). As can be seen from the first and last picture in the illustration one of the aims of the surgery is to reposition the nipple back to the level of the breast crease (also known as the inframammary fold). Top middle: To reduce the volume of the breast, the skin and breast tissue that will be removed from both the inner and outer aspect of the breast is marked together with the pedicle of breast tissue (that will keep the blood supply to the nipple intact and allow the nipple to move to its new position as well as providing projection and shape to the breast following the reduction) together with the new nipple site. Top right: The water proofing layer of the skin is removed from the pedicle (this prevents skin cells being shed inside the breast – which would lead to cyst formation).
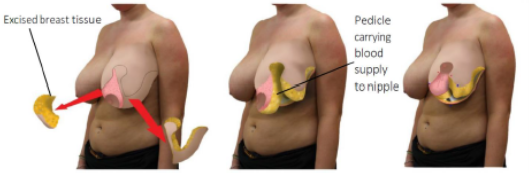
Top left: The breast tissue is excised as planned - this is the actual reduction part of the procedure - together with the creation of a hole in the skin at the site of where the nipple will sit. Top middle: The pedicle and remaining breast tissue is freed from the chest wall to allow it to be moved into its new position. Top right: The nipple is rotated into its new position using the pedicle.
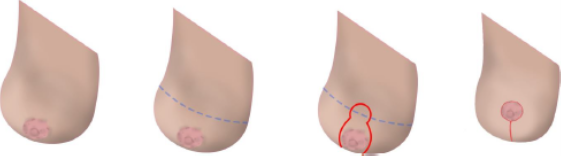
Illustration below: Short or vertical scar technique - incision and final scar location (from left to right): A large breast demonstrating nipple descent (ptosis).
The inframammary fold (IMF) is marked with a blue dashed line.
A new nipple position is marked at the level of the level of the IMF together with the skin excision lines (in red). Breast with nipple in new position (scar around nipple and running vertically down from nipple).
Choice of technique is normally the result of the discussion between yourself and your doctor and takes into account the degree of reduction you are hoping to get and what scar pattern you are happy with. Crucially and often the determining factor, is what technique will work best with your particular anatomy.
In certain cases (very large volume breasts and those in which the nipple needs to be moved very long distances) free nipple grafting is performed. This is where the nipple is removed from the breast all together and sewn into the new nipple position as a skin graft (new blood vessels grow from the raw surface of the breast tissue into the nipple over a period of days to keep it alive). This is usually done because using other techniques would leave the nipple at high risk of having insufficient blood supply and may result in death of the nipple.
There are many ways to perform a breast reduction. Your surgeon will discuss which technique they believe will work best in your case and with a view to accommodating or best meeting your own aims. It is not usual for a surgeon to explain in detail every possible technique but if you wish to discuss that in further detail/obtain further information please ask your surgeon. If there are particular goals you wish to achieve from the surgery then you need to make sure that you have discussed these with your surgeon so that they can discuss the options available to best address them.
ADDITIONAL FORMS OF SURGICAL TREATMENT
In certain circumstances liposuction can be used to perform breast reduction. When performed by itself and not as part of a surgical breast reduction procedure as described above it is not possible to move the nipple. Such procedures will decrease breast volume but will not usually improve breast shape. Liposuction tends not to work well on younger patients who have a higher proportion of glandular tissue within their breast.
ARE THERE ANY NON-SURGICAL WAYS I CAN REDUCE THE SIZE OF MY BREASTS?
Reduction in the size of your breasts can potentially be achieved through weight loss although this may not be practical for all patients and some may not see a significant change in breast size despite weight loss. Alternative approaches include physical therapy to treat pain complaints or wearing specialist undergarments to support large breasts.
WILL THE RESULTS OF SURGERY BE PERMANENT?
So long as your weight is stable the size of your breasts should remain the same following surgery. Very rarely breast size can increase but this is associated with hormonal problems and is associated either with medication or a hormone secreting tumour. Conversely if you lose weight your breast size may become smaller.
PREGNANCY FOLLOWING SURGERY
If you become pregnant following breast surgery it is likely that the outcome of your breast reduction surgery will be affected.
Importantly, breast reduction will reduce the likelihood of you being able to breast feed.
These points must be taken into consideration when making the decision to have a breast reduction.
COMPLICATIONS AND RISKS OF SURGERY
Anyone considering surgery should approach the decision with a healthy amount of respect and caution especially when the surgery is elective (or planned) and is non-essential surgery (as aesthetic or cosmetic surgery generally is).
All surgical procedures have limitations in terms of achievable outcomes and it is important that your expectations match what is possible through surgery and that you are aware of the material risks and complications. Your surgeon will have discussed these risks and complications during your consultation. It is important that you take the time to read them prior to your next consultation.
GENERAL COMPLICATIONS/RISKS
Bleeding: It is possible, though unusual, to experience a bleeding episode during or after surgery. Should post-operative bleeding occur, it may need draining surgically. If a collection of blood accumulates within the breast (a haematoma) that is small enough to not be detected clinically this may result in a spontaneous discharge from the breast at a later date (if this happens it is usually a few weeks following surgery) most small haematomas resolve spontaneously however. A haematoma can occur at any time following injury to the breast.
Seroma: A seroma can be best thought of a collection of fluid beneath the skin or within the tissue at a surgical site. If this occurs there is the possibility it will need to be drained with a needle, it may resolve itself or require an operation to drain it.
Infection: Infection is unusual after surgery. If there is a collection of fluid within the breast (a seroma or haematoma) these can become infected. Should an infection occur, additional treatment including antibiotics, hospitalization, or additional surgery may be necessary.
Scarring: All surgery leaves scars, some more visible than others. Although good wound healing after a surgical procedure is expected, abnormal scars may occur within the skin and deeper tissues. Scars may be unattractive and a different colour compared to the surrounding skin. Scar appearance may also vary within the same scar. Scars may be asymmetrical (appear different on the right and left side of the body). There is the possibility of visible marks in the skin from sutures. In some cases scars may require surgical revision or treatment. Scars can appear thick, red and raised all or part of the way along the incision line (a hypertrophic scar) or more rarely can involve tissues beyond the incision itself (and can resemble a badly healed burn), this is known as a keloid scar. Additionally, scars can tether to underlying structures or become abnormally pigmented. It is possible that additional treatments may be required for adverse scarring.
Delayed Healing: Wound disruption or delayed wound healing is possible. Some areas of the breast skin or nipple region may not heal normally and may take a long time to heal. Areas of skin or nipple tissue may die. This may require frequent dressing changes or further surgery to remove the non-healed tissue. Individuals who have decreased blood supply to breast tissue from past surgery or radiation therapy may be at increased risk for delayed wound healing and poor surgical outcome as may patients with conditions such as diabetes. Smokers have a greater risk of skin loss and wound healing complications.
Skin Discoloration / Swelling: Some bruising and swelling normally occurs following a reduction mammaplasty. The skin in or near the surgical site can appear either lighter or darker than surrounding skin. Although uncommon, swelling and skin discoloration may persist for long periods of time and, in rare situations, may be permanent. Additionally, these areas may have exaggerated responses to hot or cold temperatures. Because of changes in the pattern of blood flow within the breast brought about by the surgery it is possible to develop new blood vessels which may be visible under the skin.
Sensory changes: With any form of surgery small nerve branches that supply the skin will be cut. This can lead to patches of numbness around the surgical site. It is possible that following surgery you can develop abnormal sensation in the area where you have had surgery and this may take the form of pins and needles (known as paraesthesia), hypersensitivity or even pain in response to normal touch (known as allodynia). Such problems may be related to nerves becoming entrapped within scar tissue and further surgery may help. It may be necessary to take medication to control any such symptoms on a permanent basis. Numbness following surgery is normal and usually resolves after 12 to 18 months. It is not unusual to experience shooting pains within the breast tissue following surgery for up to a year (this is part of the healing process and represents nerve regrowth).
Suture extrusion: As well as stitches (sutures) in the skin, you will have deeper sutures to hold the breast tissue and the lower layer of the skin (known as dermis) together. These sutures are made out of material which is broken down by the body – often called dissolving sutures. Some people can develop redness in an area of the incision that is fully healed (3 or more weeks following surgery) and it appears that pus comes out. This is the body’s response to the stitch and the ‘pus’ represents the white blood cells trying to dissolve the suture (causing localized inflammation but without infection). Such areas are normally managed with simple dressings. It is possible to develop multiple suture extrusions at the same time or at different times during the healing process.
Allergic Reactions: Local allergies to tape, suture material and glues, blood products, topical preparations or injected agents can cause skin reactions. Serious systemic reactions including shock (anaphylaxis) may occur to drugs used during surgery and prescription medications. Allergic reactions may require additional treatment and can result in severe illness or death. Often, they result in minor irritation/discomfort and resolve reasonably quickly.
Deep vein thrombosis, cardiac and pulmonary complications: Any procedure requiring general anaesthesia increases the risk of the formation of blood clots in the legs. Such clots can dislodge and move to the lungs, causing shortness of breath and strain on the heart. Such clots can potentially be fatal. If you experience shortness of breath, chest pains or palpitations (abnormal heart beats) following your surgery it is important you seek medical advice immediately.
Blood Transfusion: Blood loss during surgery may require treatment with a blood transfusion. It is possible for viral transmission to occur with such treatment (HIV, hepatitis, and others). Having a blood transfusion can result in a transfusion reaction that can cause serious illness.
COMPLICATIONS SPECIFIC TO BREAST REDUCTION SURGERY
Nipple necrosis: If there is any problem with the blood supply to the nipple (because the nipples have had to be moved a long way), this may affect the healing and even the survival of the nipples. In the worst-case scenario the entire nipple may die. Otherwise, part of the nipple may form a scab, which will eventually heal underneath. If you are unlucky enough for this to happen, you may require revision surgery in the future to address poor scarring or to reconstruct a new nipple for you.
Skin and fat necrosis: If the blood supply to the skin is insufficient following surgery (which can be for a variety of reasons) it can necrose (die). If this happens the skin will form an eschar (scab) which may need to be removed surgically. Dressings are likely to be required for a period of time and further surgery may be needed to correct adverse scars. The areas of skin most susceptible to wound healing problems following breast reduction surgery are at the ‘T’ junctions (where the vertical scar joins the nipple and where it joins the breast crease scar). If there is inadequate blood supply to the breast tissue (which is composed in a large part by fat cells) this too can die (and be replaced by scar tissue). This may produce areas of firmness within the breast. Fat necrosis may also result in discharge of liquid from the surgical incision due to fat liquification. Additional surgery to remove areas of fat necrosis may be necessary. If an area of fat necrosis were to become infected it would require further treatment with antibiotics or surgery. There is the possibility of contour irregularities in the skin that may result from fat necrosis. The larger your breasts and the greater your body mass index (BMI) the more at risk you are of this complication).
Changes in nipple and skin sensation: You may experience either complete loss of or a decrease in sensitivity of the nipples and the skin of your breast. If you are having free nipple grafts (where the nipple is completely removed from the breast and sewn back on) as part of your breast reduction procedure your nipples will lose sensation. Changes in sensation may affect sexual response or the ability to breast feed a baby.
Skin Contour Irregularities: Contour and shape irregularities may occur after reduction mammaplasty. Visible and palpable wrinkling may occur (and this is a particular risk with vertical scar breast reduction). Residual skin irregularities at the ends of the incisions or “dog ears” are always a possibility when there is excessive redundant skin. This may improve with time, or you may elect to have this surgically corrected.
Firmness: Excessive firmness of the breast can occur after surgery due to internal scarring or fat necrosis. The occurrence of this is not predictable. If an area of fat necrosis or scarring appears, this may require biopsy or additional surgical treatment.
Damage to Deeper Structures: There is the potential for injury to deeper structures including nerves, blood vessels, muscles, and lungs (leading to deflation of the lung known as a pneumothorax) during breast reduction surgery. Injury to deeper structures may result in temporary or permanent loss of function of the structure damaged.
You may need to define with your surgeon which of these complications (if they occur) will be addressed without further cost to you. Any acute complication is likely to be dealt with and addressed at no cost to you but you may wish to discuss this or clarify it with your surgeon.
ASYMMETRY OF THE BREASTS
Everyone is different on the right-hand side of their face and body compared to the left and pre-existing asymmetry between breasts will influence the outcome of your surgery.
Asymmetry of the breast can result in any of the following:
Nipple asymmetry: The shape, size and position of the nipple on the breast may differ between sides following surgery.
Scar asymmetry: The shape, length and position of the scars between the right and left breasts is likely to be different (and will reflect any pre-operative differences in breast dimensions).
Breast size and shape: Breast shape and volume will not be identical following breast reduction surgery.
Breast position on the chest wall: The footprint of the breast on the chest wall – its position on the ribcage - is fixed. It is not possible to alter the position of the breast with breast reduction surgery and any pre-existing asymmetry between the sides will be present following the operation.
BREAST SIZE
Although a reduction in breast size can be guaranteed following surgery, specifying the exact cup size your breasts will be following your operation is not possible. You should not enter into the surgery with the expectation that you will achieve a particular bra size. It is important to realise and fully appreciate that you may not achieve your exact goals following breast reduction surgery. Additionally, it is important to understand that a minority of patients feel that their breasts are still too large following surgery (and that in such cases further reductions in size may not technically be possible).
BREAST SHAPE
Breast reduction surgery aims to improve breast shape by repositioning the nipple and reducing sagging of the soft tissues. By reducing the weight of the breast after the reduction there is decreased pull on the soft tissues so the tendency to stretch or sag is less. However, there will be a change in breast shape over time following surgery as gravity exerts its pull on the remaining tissue. This usually means the breast changing from a cone or conical shape to a more natural tear dropped shape. The final shape of the breast is determined by the extent of support to the breast tissue offered by the skin and the scar tissue that forms internally. This varies from patient to patient so is not predictable.
The pre-operative shape of your breast footprint will have a big part in determining the shape of the breasts post reduction surgery. If you have a naturally wide breast foot print then the your breast will have a tendency to have a square or flatter appearance in the lower pole post reduction whereas patients with a breast foot print that does not extent onto the side of the rib cage will tend to get a rounder lower pole post breast reduction surgery.
Likewise, the distribution of breast tissue volume within the breast will also have an impact on outcome of the surgery. If you have a significant amount of breast tissue above the level of the nipple you will have a fuller upper pole of the breast after your breast reduction procedure and this will not be reduced by the procedure (as the volume reduction is primarily in the lower pole of the breast).
SPECIFIC HEALTH FACTORS AFFECTING THE OUTCOME OF BREAST REDUCTION SURGERY
Body mass index: Research has shown that the higher your body mass index (BMI) the more likely you are to have a complication post-surgery. Achieving the healthiest BMI possible prior to surgery is always recommended.
https://www.nhs.uk/live-well/healthy-weight/bmi-calculator/
Smoking: Smoking or vaping with a nicotine vape (or using a nicotine patch or gum) reduces blood flow to the tissues and results in poorer scarring, wound healing, higher risk of nipple loss and is associated with a higher rate of complications in general. You are advised to stop smoking 6 weeks prior to surgery and to refrain from smoking thereafter.
Medications: Certain medications can interfere with wound healing and increase the likelihood of infections following breast reduction surgery. It is important that you inform your surgeon of all the medications you are on.
Diabetes: Diabetes affects immune system function, as well as tissue perfusion (blood flow) and wound healing. You are at higher risk for developing complications following surgery if you suffer with diabetes.
ADDITIONAL CONSIDERATIONS RELATING TO BREAST REDUCTION SURGERY
Breast feeding: Having a breast reduction will reduce your chances of being able to breast feed. The chance of being able to breast feed following surgery varies depending on the exact surgical technique. If this is important to you then it is essential to ask your surgeon for further details on how they anticipate your chances of successfully breast feeding will be affected by the surgery.
Surgical plan: Although a pre-operative plan will have been discussed prior to the operation, there are multiple ways of undertaking an individual procedure. Each technique has been developed to achieve the same end result (though may result in differing scar patterns). It may sometimes be necessary to alter the initial plan discussed with you at the time of operation due to anatomic considerations that become apparent during the course of the surgery. Your surgeon will discuss with you what may be subject to change or what these changes may be - this varies between different types of procedure.
Unsatisfactory Result: Although good results are always aimed for, they cannot be guaranteed. You may be disappointed with the results of breast reduction surgery. Asymmetry in nipple location, unanticipated breast shape and size, loss of function, wound disruption, poor healing, and loss of sensation may occur after surgery. Unsatisfactory surgical scar location or visible deformities at the ends of the incisions (dog ears) may occur. Liposuction may be necessary to thin breast tissue that is outside of the normal surgical location for breast reduction surgery, and this may be classed as an additional procedure and incur an extra charge. It may be necessary to perform additional surgery to attempt to improve your results.
Although the risks and complications occur infrequently, the above risks are particularly associated with breast reduction surgery. In addition to the risks and complications outlined above there are others that can and do occur, though these are even more uncommon. The outcomes of surgery and medicine are influenced by many factors beyond the control of your surgeon and as such cannot be predicted.
Disclaimer
This document is designed to give you useful information. It is not advice on your specific needs and circumstances. It does not replace the need for you to have a thorough consultation, so you should get advice from a suitably qualified medical practitioner. We – The BAAPS and BAPRAS – have no liability for any decision you make about the surgery you decide to have.
